Painkillers: New Guidlines
Opioid painkillers such as OxyContin and Vicodin are now prescribed to as much as 4% of the U.S. population — 250 million prescriptions — with their use quadrupling since 1999. Some 1.9 million Americans are now addicted to, or dependent on, the painkillers. And from 1999 to 2014, about 165,000 people died of overdoses. Almost all of the opiate-related drugs on the market for pain are as addictive as heroin.
According to the National Institute on Drug Abuse (NIDA), the abuse of and addiction to opioids such as heroin, morphine, and prescription pain relievers is a serious global problem that affects the health, social, and economic welfare of all societies. It is estimated that between 26.4 million and 36 million people abuse opioids worldwide, with an estimated 2.1 million people in the United States suffering from substance use disorders related to prescription opioid pain relievers in 2012 and an estimated 467,000 addicted to heroin. The consequences of this abuse have been devastating and are on the rise. For example, the number of unintentional overdose deaths from prescription pain relievers has soared in the United States, more than quadrupling since 1999. There is also growing evidence to suggest a relationship between increased non-medical use of opioid analgesics and heroin abuse in the United States.
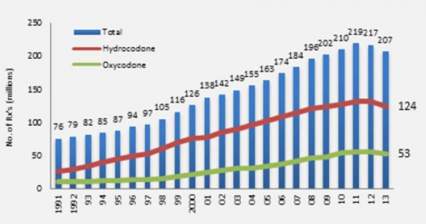
Increase in Opioid Prescriptions 1991-2013
Opioid medications can produce a sense of well-being and pleasure because these drugs affect brain regions involved in reward. People who abuse opioids may seek to intensify their experience by taking the drug in ways other than those prescribed. For example, extended-release oxycodone is designed to release slowly and steadily into the bloodstream after being taken orally in a pill; this minimizes the euphoric effects. People who abuse pills may crush them to snort or inject which not only increases the euphoria but also increases the risk for serious medical complications, such as respiratory arrest, coma, and addiction. When people tamper with long-acting or extended-release medicines, which typically contain higher doses because they are intended for release over long periods, the results can be particularly dangerous, as all of the medicine can be released at one time. Tampering with extended release and using by nasal, smoked, or intravenous routes produces risk both from the higher dose and from the quicker onset.
The Centers for Disease Control released a dozen opioid prescription guidelines in the Journal of the American Medical Association (JAMA). They will not have the power of law but will guide insurance company recommendations to doctors and Veterans Administration prescriptions for retired military patients, with the aim of curbing dangerous prescribing practices. "Primary care clinicians find managing chronic pain challenging," according to JAMA, and "evidence of long-term efficacy of opioids for chronic pain is limited. Opioid use is associated with serious risks, including opioid use disorder and overdose."
The guidelines are based on three principles. First, opioids should be a last option for these patients, with aspirin-related drugs and exercise preferred. Second, when given, doses should start out low and only increase slowly. Third, patients should be monitored and a plan for getting them off the drugs should start with their prescription. The guidelines also call for getting naloxone, a drug used to counteract overdoses, into the hands of more doctors, nurses, police, and emergency personnel.
Never Underestimate the Power of a Single Intervention
A few minutes of counseling in a primary care setting could go a long way toward steering people away from risky drug use -- and possibly full-fledged addiction, a UCLA-led study suggests. (Primary care refers to family physicians and other non-psychiatrists who provide most of our medical care.)
People who participated in the Quit Using Drugs Intervention Trial, or Project QUIT, which was a randomized controlled trial conducted in medical clinics, reduced their risky drug use by one-third when primary care doctors and health coaches provided them with brief interventions during a routine visit and follow-up phone calls.
Risky drug use is defined as the casual, frequent or binge use of illicit drugs such as cocaine, heroin and methamphetamine, or the misuse of prescription medications, without showing physiological or psychological signs of addiction. There are an estimated 68 million such drug users in the United States. These people are at risk not only for becoming addicts, but suffering attendant physical, mental health and social problems.
The study, published today in the peer-reviewed journal Addiction, is the first to demonstrate that a brief intervention led by a primary care physician can significantly reduce risky drug use among patients.
We Don't Plan to Become Addicts or Alcoholics
Most of the patients I (Dr. Talmadge) see in practice did not plan to become addicted to drugs. Casual use introduces powerful chemicals in the brain, and many of us then have our brains hijacked by these chemicals. As described in the HBO special on addictions, the human brain is an extraordinarily complex and fine-tuned communications network containing billions of specialized cells (neurons) that give origin to our thoughts, emotions, perceptions and drives. Often, a drug is taken the first time by choice to feel pleasure or to relieve depression or stress. But this notion of choice is short-lived. Why? Because repeated drug use disrupts well-balanced systems in the human brain in ways that persist, eventually replacing a person's normal needs and desires with a one-track mission to seek and use drugs. At this point, normal desires and motives will have a hard time competing with the desire to take a drug.
How Does the Brain Become Addicted?
As described in the HBO documentary, typically it happens like this:
-A person takes a drug of abuse, be it marijuana or cocaine or even alcohol, activating the same brain circuits as do behaviors linked to survival, such as eating, bonding and sex. The drug causes a surge in levels of a brain chemical called dopamine, which results in feelings of pleasure. The brain remembers this pleasure and wants it repeated.
-Just as food is linked to survival in day-to-day living, drugs begin to take on the same significance for the addict. The need to obtain and take drugs becomes more important than any other need, including truly vital behaviors like eating. The addict no longer seeks the drug for pleasure, but for relieving distress.
-Eventually, the drive to seek and use the drug is all that matters, despite devastating consequences.
-Finally, control and choice and everything that once held value in a person's life, such as family, job and community, are lost to the disease of addiction.
What brain changes are responsible for such a dramatic shift?
Research on addiction is helping us find out just how drugs change the way the brain works. These changes include the following:
Reduced dopamine activity. We depend on our brain's ability to release dopamine in order to experience pleasure and to motivate our responses to the natural rewards of everyday life, such as the sight or smell of food. Drugs produce very large and rapid dopamine surges and the brain responds by reducing normal dopamine activity. Eventually, the disrupted dopamine system renders the addict incapable of feeling any pleasure even from the drugs they seek to feed their addiction.
Altered brain regions that control decisionmaking and judgment. Drugs of abuse affect the regions of the brain that help us control our desires and emotions. The resulting lack of control leads addicted people to compulsively pursue drugs, even when the drugs have lost their power to reward.
The disease of addiction can develop in people despite their best intentions or strength of character. Drug addiction is insidious because it affects the very brain areas that people need to "think straight," apply good judgment and make good decisions for their lives. No one wants to grow up to be a drug addict, after all.
The addiction study cited above has some limitations. The results are based on participants' self-reporting, so the study may suffer from reporting bias. However, researchers found that based on urine testing, under-reporting of drug use was low. Additional limitations: not everyone in the clinic waiting rooms agreed to participate, which could impact the study's generalizability; there was some attrition during the study, though the 75 percent participation rate at follow-up compares to other studies of low income patients and drug use; and the three month follow up was relatively short.
There is a need for larger trials to gauge the QUIT program's effectiveness, but based on these findings the project appears to have the potential to fill an important gap in care for patients who use drugs, particularly in low-income communities, Gelberg said.
Read the entire report and article by clicking here.
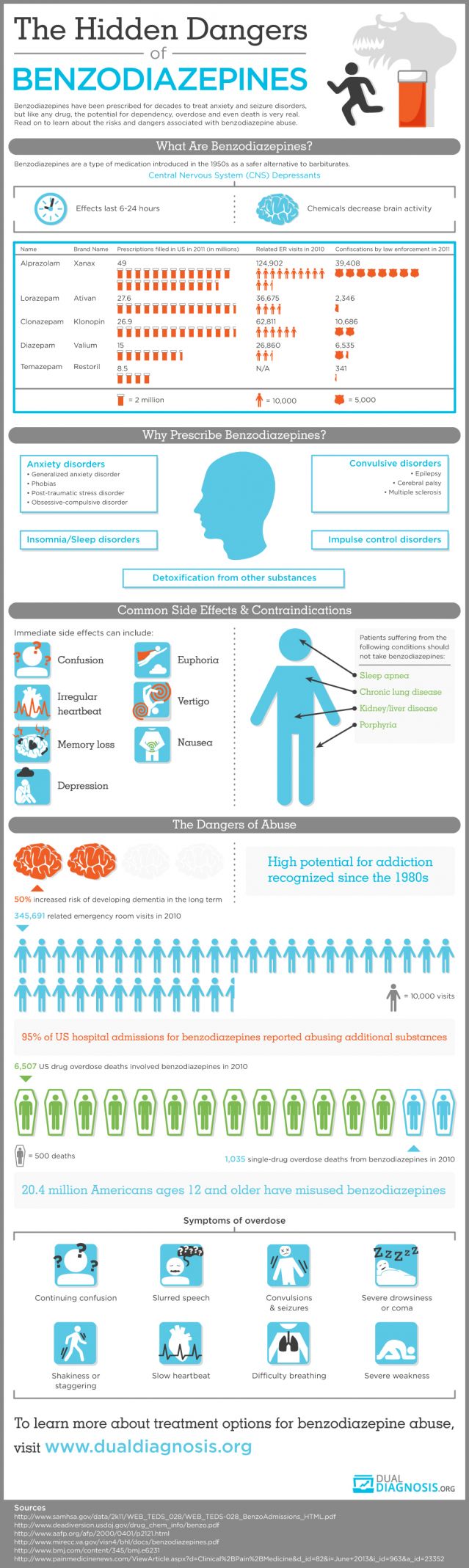
One Nation, Under Sedation
Houston, we have a problem. For the full story, click here.
The distinguished addiction specialist Charles O'Brien, M.D., authored a paper in 2005 discussing the risks of benzodiazepine abuse. The summary of his article states: "Although benzodiazepines are invaluable in the treatment of anxiety disorders, they have some potential for abuse and may cause dependence or addiction. It is important to distinguish between addiction to and normal physical dependence on benzodiazepines. Intentional abusers of benzodiazepines usually have other substance abuse problems. Benzodiazepines are usually a secondary drug of abuse-used mainly to augment the high received from another drug or to offset the adverse effects of other drugs. Few cases of addiction arise from legitimate use of benzodiazepines. Pharmacologic dependence, a predictable and natural adaptation of a body system long accustomed to the presence of a drug, may occur in patients taking therapeutic doses of benzodiazepines. However, this dependence, which generally manifests itself in withdrawal symptoms upon the abrupt discontinuation of the medication, may be controlled and ended through dose tapering, medication switching, and/or medication augmentation. Due to the chronic nature of anxiety, long-term low-dose benzodiazepine treatment may be necessary for some patients; this continuation of treatment should not be considered abuse or addiction."
Painkiller Overdoses On the Rise
This news isn’t shocking to those of us who encounter addiction daily, but it’s in the headline today at USA Today. Other items of note from today’s paper:
With nearly 44,000 deaths a year, more Americans today die from drug overdoses than from car accidents or any other type of injury. Many of these deaths could be prevented if patients had better access to substance abuse therapy, experts say. Yet people battling addiction say that treatment often is unavailable or unaffordable.
Only 11% of the 22.7 million Americans who needed drug or alcohol treatment in 2013 actually got it, according to the Substance Abuse and Mental Health Services Administration. While some of those who went without care did so by choice, at least 316,000 tried and failed to get treatment.
"We know addiction treatment saves lives, reduces drug use, reduces criminal activity and improves employment," says Paul Samuels, president and director of the Legal Action Center, which advocates on behalf of people with HIV or addiction. "The data is there, the evidence is in, but our public policy has not caught up with the science."
Meanwhile, the crisis is getting worse, says Thomas Frieden, director of the Centers for Disease Control and Prevention. The death rate from drug overdoses more than doubled from 1999 to 2013, according to the CDC. The bulk of these deaths involve opiates, a class of pain killers that includes morphine and Oxycontin.
Injection drug use has fueled an outbreak of HIV in rural Indiana, a nationwide surge in hepatitis C infections, and an increase in the number of babies born addicted to drugs. States have responded to the surge in overdose deaths by expanding access to naloxone, a fast-acting rescue drug that can reverse the effects of an opiate overdose. Indiana lawmakers also voted to allow needle exchange programs in communities facing a public health crisis related to injection drug use. While those approaches are welcome, they don't treat the underlying addiction.
The wait for a spot in a detoxification program ranges from days to weeks, and it can be very expensive. As I say elsewhere here on my site, it's also true that not all treatment is really good treatment. Consumers are disadvantaged twice. Not only is treatment hard to find in the first place, but it's hard to know what constitutes a good treatment program. I have some comments about this on my FAQ page and on my Philosophy page.