Painkillers: New Guidlines
Opioid painkillers such as OxyContin and Vicodin are now prescribed to as much as 4% of the U.S. population — 250 million prescriptions — with their use quadrupling since 1999. Some 1.9 million Americans are now addicted to, or dependent on, the painkillers. And from 1999 to 2014, about 165,000 people died of overdoses. Almost all of the opiate-related drugs on the market for pain are as addictive as heroin.
According to the National Institute on Drug Abuse (NIDA), the abuse of and addiction to opioids such as heroin, morphine, and prescription pain relievers is a serious global problem that affects the health, social, and economic welfare of all societies. It is estimated that between 26.4 million and 36 million people abuse opioids worldwide, with an estimated 2.1 million people in the United States suffering from substance use disorders related to prescription opioid pain relievers in 2012 and an estimated 467,000 addicted to heroin. The consequences of this abuse have been devastating and are on the rise. For example, the number of unintentional overdose deaths from prescription pain relievers has soared in the United States, more than quadrupling since 1999. There is also growing evidence to suggest a relationship between increased non-medical use of opioid analgesics and heroin abuse in the United States.
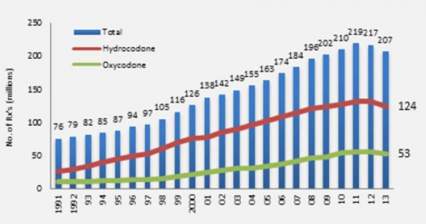
Increase in Opioid Prescriptions 1991-2013
Opioid medications can produce a sense of well-being and pleasure because these drugs affect brain regions involved in reward. People who abuse opioids may seek to intensify their experience by taking the drug in ways other than those prescribed. For example, extended-release oxycodone is designed to release slowly and steadily into the bloodstream after being taken orally in a pill; this minimizes the euphoric effects. People who abuse pills may crush them to snort or inject which not only increases the euphoria but also increases the risk for serious medical complications, such as respiratory arrest, coma, and addiction. When people tamper with long-acting or extended-release medicines, which typically contain higher doses because they are intended for release over long periods, the results can be particularly dangerous, as all of the medicine can be released at one time. Tampering with extended release and using by nasal, smoked, or intravenous routes produces risk both from the higher dose and from the quicker onset.
The Centers for Disease Control released a dozen opioid prescription guidelines in the Journal of the American Medical Association (JAMA). They will not have the power of law but will guide insurance company recommendations to doctors and Veterans Administration prescriptions for retired military patients, with the aim of curbing dangerous prescribing practices. "Primary care clinicians find managing chronic pain challenging," according to JAMA, and "evidence of long-term efficacy of opioids for chronic pain is limited. Opioid use is associated with serious risks, including opioid use disorder and overdose."
The guidelines are based on three principles. First, opioids should be a last option for these patients, with aspirin-related drugs and exercise preferred. Second, when given, doses should start out low and only increase slowly. Third, patients should be monitored and a plan for getting them off the drugs should start with their prescription. The guidelines also call for getting naloxone, a drug used to counteract overdoses, into the hands of more doctors, nurses, police, and emergency personnel.